A Coast That Heals: Mental Health Stories from Kenya’s Shores
Reading Time: 5min
By the Indian Ocean, where the waves sweep over Diani’s white sands, Malindi’s bustling streets, and Mtwapa’s busy market corners, a quiet revolution is unfolding. For decades, mental health in Kenya was whispered about behind closed doors, shrouded in stigma and superstition. Families hid loved ones, fearful of judgment. Problems once called “madness” or “bewitchment” went unaddressed, leaving a generation to struggle in silence.
Today, that is changing. From Voi to Kilifi, from Taita Taveta to Mtwapa, communities are proving that healing is possible, stigma can be dismantled, and hope is not just a word—it is a lived reality.
Shamiri in Voi: Teaching Teens to Thrive
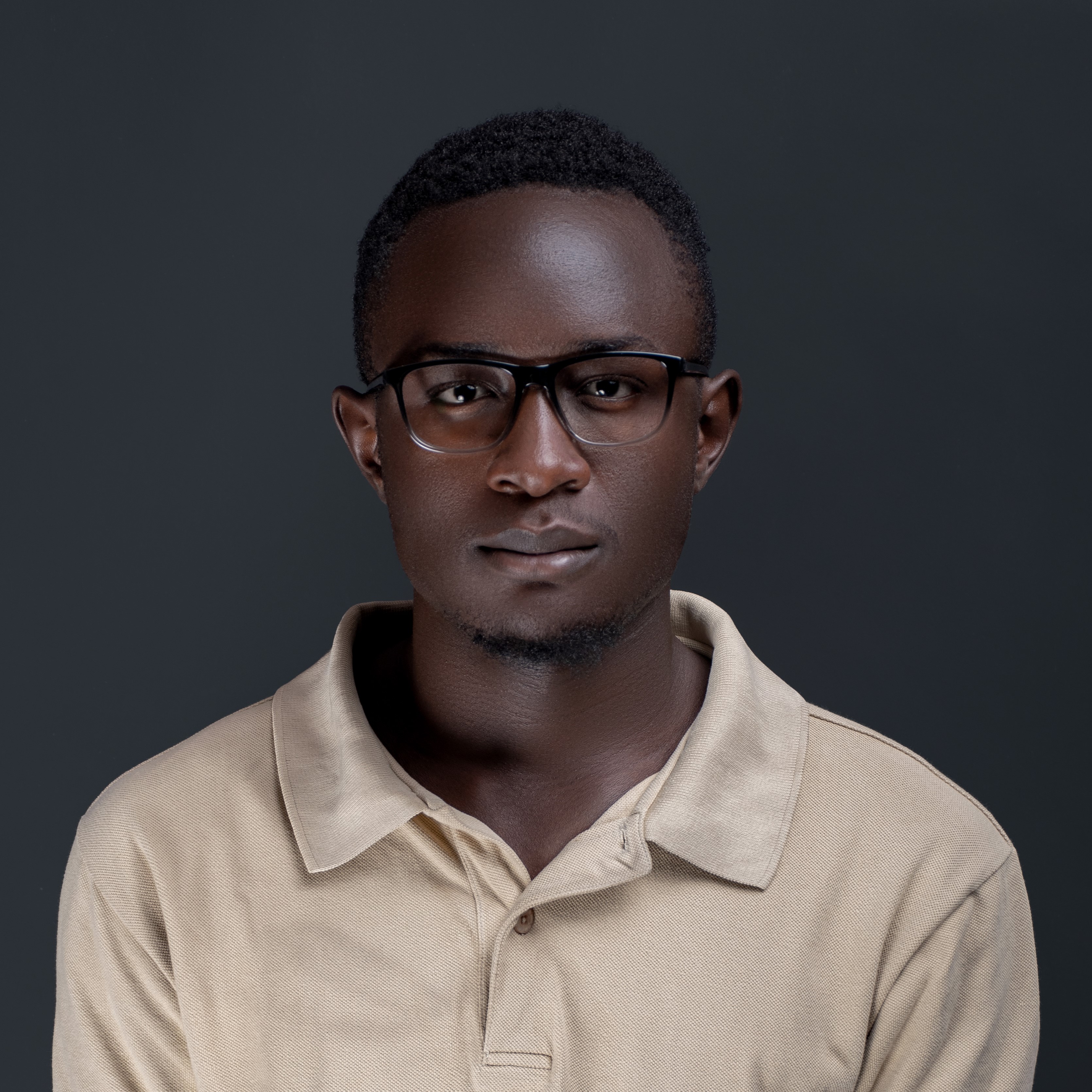
At Voi Girls’ Secondary School, Form Three student Brian Mwangi sits under a jacaranda tree and talks about the shift in his life.
“I used to think I was failing at everything—school, friends, life,” he says, staring at the ground. “Shamiri taught me that small changes in how I think about myself can actually make a difference.”
Shamiri (Kiswahili for “thrive”) is a program designed by researchers from the University of Nairobi and implemented in several schools across Taita Taveta County. Over four weeks, students learn gratitude, affirm their personal values, and practice growth mindset strategies—the idea that abilities can be developed.
What makes Shamiri remarkable is what it avoids: clinical labels. There’s no talk of “mental illness” or “therapy.” Instead, it focuses on character strengths and life skills. Teachers like Esther Nthiga at Voi Boys’ Secondary noticed immediate changes.
“Students who were withdrawn started participating in class, laughing, sharing ideas. The program gave them language for feelings they didn’t know how to express,” she recalls.
For students like Brian, who lost his father to alcoholism and has lived with anxiety since early adolescence, Shamiri offered tools to navigate both school and home life. “Now I can tell my mother when I’m feeling low instead of keeping it inside,” he says.
The program’s success lies in its cultural sensitivity: it meets students where they are, avoiding the fear and stigma often triggered by terms like “mental illness.”
Taita Taveta: A Community Learning to Flourish
Up the hills of Taita Taveta, in villages from Wundanyi to Mwatate, mental health is being addressed not just in clinics but in homes and community halls. The Flourishing Communities Model (FCM), pioneered by local NGOs, links economic empowerment with psychological wellbeing.
Joseph Mutiso, 19, was once street-connected in Voi. “I used to wander the streets with nothing,” he says. “Now I run a small vegetable stall with my mother. I can support my siblings and talk about what happened to me without shame.”
The FCM works in phases: first, building social trust; then, supporting group savings and micro-loans; finally, addressing collective trauma and teaching skills like stress management and problem-solving. Families who had been isolated, distrustful, or struggling economically are now participating in weekly community meetings, supporting one another through both practical challenges and emotional wounds.
Elizabeth Kilonzo, a mother in Wundanyi, recounts how the program helped her teenage son, who had attempted suicide after repeated bullying.
“The counselors didn’t treat him like he was broken. They helped him see his own worth, and now he teaches other young people in the village about coping and resilience,” she says.
Similarly, in Mwatate, young mothers struggling with postnatal depression attend peer support groups facilitated by community health volunteers. Mercy Njenga, 27, says:
“I felt ashamed when I couldn’t care for my baby properly. Talking to others who understood me made me feel human again. I didn’t feel like I was failing anymore.”
Lesson: Mental health is inseparable from the health of the community. Economic empowerment, social cohesion, and trauma-informed support can transform lives faster than clinic-based interventions alone.
Mombasa and Malindi: Youth, Substance Abuse, and Mental Health
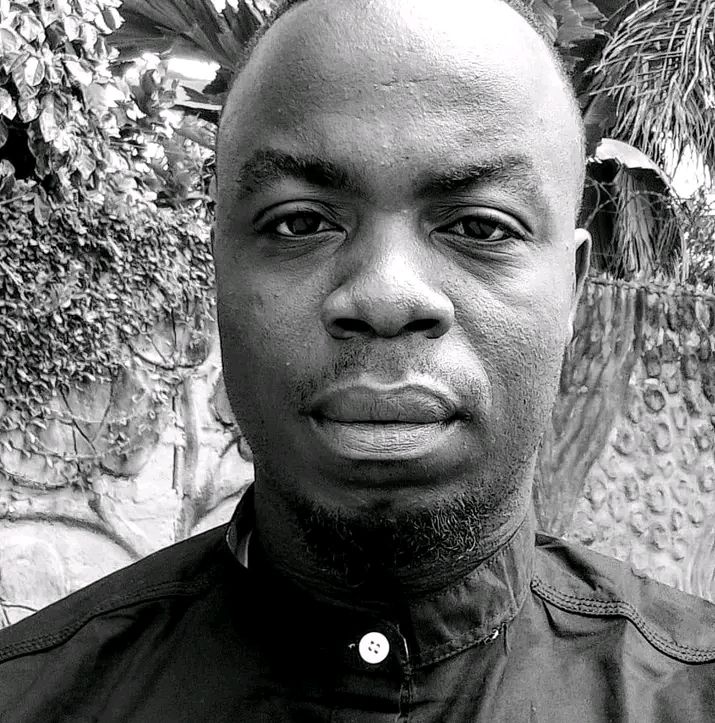
In Mtwapa, 21-year-old Hassan Ali navigates the crowded streets selling second-hand clothes. He dropped out of school two years ago after struggling with anxiety and depression that no one recognized. “I started smoking bhang and drinking alcohol to calm my mind,” he admits. “At first, it helped me sleep. Then it controlled me.”
Hassan is part of a growing movement of coastal youth supported by MindTheMap, a Nairobi-based mental health initiative now working in Mombasa and Kilifi counties. The program trains youth leaders to facilitate peer discussions on substance abuse, mental health, and coping strategies.
“Before, I thought I was alone,” says Hassan. “Now I know other people struggle too. We talk, we support each other. I’m starting to sleep better, think better, and even plan to go back to school.”
Kilifi County tells a similar story. In Mariakani, Zainab Omar, a youth leader, works with teens facing alcohol abuse. She recalls 17-year-old Joseph Mwende:
“He started drinking after losing his father. His mother didn’t know how to help. Through our group, he learned to talk about his feelings, and we connected him with counseling and vocational skills training. Now he’s running a small tailoring business and helping his mother with income.”
These programs are quiet revolutions. They show that community-driven interventions—peer support, mentoring, vocational skills—can tackle the roots of distress while breaking down stigma.
Legal Change: Compassion over Punishment
For years, the law criminalized attempted suicide, adding fear to trauma. Grace Mwikali, 29, from Malindi, survived an attempt in 2019.
“I was terrified of telling anyone what happened because I could be arrested,” she says. “Now, after the 2025 High Court ruling, I can seek help without fear. I can survive without shame.”
This ruling, championed by the Kenya National Commission on Human Rights and the Kenya Psychiatric Association, marked a shift from punishment to care, sending a clear message: emotional pain deserves empathy, not prosecution.
The Coast’s Natural Ally: Blue Health
One unique advantage of the coast is its environment. Growing research into “Blue Health” shows that time near water reduces stress and boosts mood. In Malindi, Mariam Ali, 22, practices mindfulness on the beach to manage anxiety. “The waves help me focus on my breathing. I feel calmer than in my room,” she says.
In Diani, Ahmed Juma runs surf therapy sessions for at-risk youth. “It’s not just about surfing,” he explains. “It’s about learning balance, patience, and presence. The ocean teaches lessons about resilience.”
The Road Ahead
These stories are victories, but the journey is far from complete. Stigma persists, resources are thin, and much of the coast remains underserved. Programs like Shamiri, FCM, and youth-led mental health initiatives are beacons, but they need support to reach more schools, villages, and towns.
The lessons are clear:
Strength-based, culturally sensitive interventions work.
Mental health is linked to economic and social wellbeing.
Compassionate laws protect and empower those in crisis.
Community and environment are powerful healing tools.
From the waves of Diani to the streets of Mtwapa, the conversation on mental health is no longer a whisper. It rises with the tide, a chorus of voices saying:
“You are not alone. There is hope. Healing is possible.”
If you or someone you know is struggling, please reach out. You can contact the Kenya National Mental Health helpline or seek support from local community health workers. Your story matters.